Failed Back Surgery Syndrome
How Can Back Surgery “Fail” and What Are My Options if it Does?
Is Back Surgery the Best Way to Cure Back Pain?
Unless a patient is experiencing severe or progressive complications from back pain (such as symptoms of weakness, or loss of bowel or bladder control), there’s no evidence that early surgery will improve conditions such as disc prolapse or spinal stenosis[i].
The American Pain Society recommends that surgery be discussed as an option only after a patient has suffered from disabling, non-radicular low pack pain for a minimum of 1 year due to the significant risks associated with surgery. Even then, the Society recommends a thorough discussion of the risks and benefits, and full consideration of the evidence that alternative therapies might be just as effective as surgery.
Learn More about Back Pain Treatments
How Common is Back Pain?
Low back pain is one of the most common conditions in adults. More than one in three adults say back pain impacts everyday activities, including sleep, and back pain is one of the most common conditions that send us to our doctors every year. Most back problems respond to non-surgical alternatives (such as anti-inflammatory medications, chiropractic adjustment, massage, injections, and physical therapy).
Back pain is a complex issue, and spine surgery has significant risk of complications and so is often a last resort. Some doctors may recommend surgery if back pain fails to respond to conventional treatments and a patient’s life is disrupted by severe pain.
Up to 40% of surgery patients report ongoing pain, or pain as a result of their back surgery, with each subsequent procedure increasing the chance of ongoing pain. This phenomenon is referred to as “Failed Back Surgery Syndrome” and to understand it, we must first understand why back surgery may be recommended and what it involves.
What are the Types of Back Surgery?
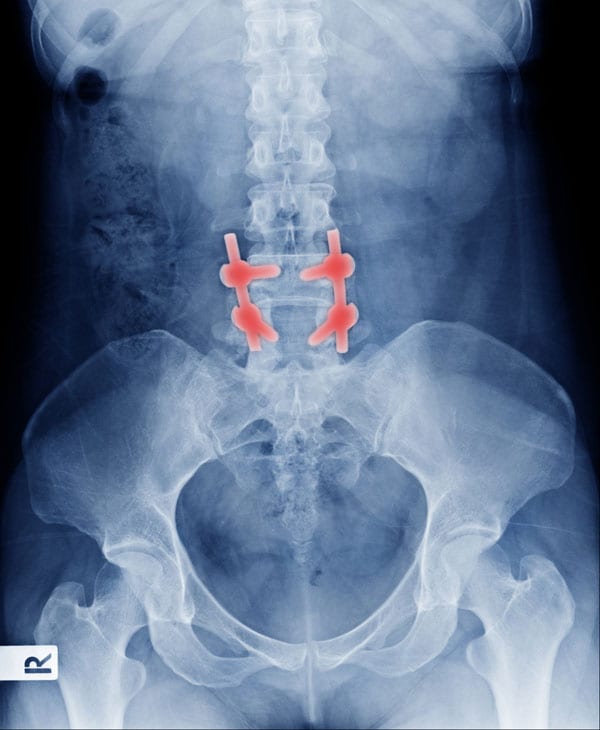
Depending on the condition, back surgery aims to relieve pressure of discs or joints contributing to narrowing of the space where the spinal nerve roots exit the spinal canal, or to decompress the central spinal canal itself. Sometimes surgery can involve removal of the entire disc and fusing the bones with or without placement of a spacer in place of the disc. There is also an option in a small subset of patients for an artificial disc replacement.
Different types of back surgery include:
Artificial disc replacement is a newer alternative to fusion. A prosthetic disc could help preserve normal range of motion and spine mechanics. This could reduce the long-term degenerative changes in adjacent vertebral segments following spinal fusion. However, the evidence suggests that the efficacy of this approach is similar to that of spinal fusion.
What is Failed Back Surgery Syndrome?
Failed Back Surgery Syndrome is an umbrella term that covers a group of conditions that cause persistent back pain (with or without sciatica) following one or more spine surgeries[ii]. An estimated 30-40% of back surgery patients can suffer from Failed Back Surgery syndrome in the long term. Each successive surgery after the first increase this estimate, with up to 85% of patient reporting Failed Back Surgery Syndrome symptoms after four surgeries[iii].
How Does Back Surgery “Fail”?
What are the Causes of Failed Back Surgery Syndrome?
Failed Back Surgery Syndrome symptoms are generally caused by residual scarring, inflammation, or anatomical abnormalities that alter the normal mechanics of the spine and create pressure on the nerves. A more comprehensive list of causes includes:
- Psychological and mood factors (depression, anxiety, or other mood disorders) and tobacco use may decrease response to surgical and non-surgical treatment
- Obesity increases risk of intraoperative and postoperative complications
- Scar tissue formation after back surgery
- Recurrent or persistent disc herniation
- Spinal stenosis
- Post operative infection
- Epidural post-operative fibrosis
Can Failed Back Surgery Syndrome be Treated?
Treatments or Failed Back Surgery Syndrome follow the same basic progression as treatments for acute or chronic back pain. The short-term goal is to reduce the pain from the syndrome, with a long-term goal of correcting dysfunction in spine mechanics and increasing core strength to reduce the stress on the spine structure.This process may include one or more of the treatments listed on the right.
What is the Recovery Time from Failed Back Surgery Syndrome?
Given the complex nature of Failed Back Surgery Syndrome’s causes and symptoms, recovery time varies widely from patient to patient. The recovery time depends on the nature of the pain, the condition of the patient, and how involved the patient chooses to be in their recovery process. Spinal Cord Stimulation has been shown to have lasting relief from Failed Back Surgery Syndrome symptoms, with up to 53% of patients reporting sustained pain relief and satisfaction, even years after their implant, while only 22% of patients who opted for other treatments reported similar success in long-term follow-up.
When Can I Return to Work After Failed Back Surgery Syndrome?
Although the time frame for when a Failed Back Surgery Syndrome patient can return to work varies as widely as the projected recovery time. However, most people who leave work on disability for failed back surgery syndrome struggle to return to their full-time jobs. However, a five-year follow-up study showed that 25% of disabled patients receiving Spinal Cord Stimulation treatment for Failed Back Surgery symptoms were able to return to work.


